Healthcare RCM: Optimize Revenue Cycle Administration for Better Results
Healthcare RCM: Optimize Revenue Cycle Administration for Better Results
Blog Article
Discover Exactly How Health Care RCM Processes Transform Administrative Tasks Into Seamless Operations
In the ever-evolving landscape of healthcare, Income Cycle Management (RCM) procedures have arised as a crucial pressure in transforming administrative jobs into smooth procedures. By utilizing innovative innovation and refined approaches, RCM offers an advanced approach to taking care of client registration, payment, and claims processing. The solutions to these concerns are essential for comprehending the future of healthcare administration.
Comprehending Medical Care RCM
Profits Cycle Monitoring (RCM) in healthcare is an important procedure that makes sure the economic wellness of clinical institutions by looking after the whole lifecycle of client solution revenue. It incorporates numerous administrative and clinical features, starting from the preliminary scheduling of a clinical consultation to the eventual collection of repayment for solutions provided. Healthcare RCM. RCM is crucial in managing the complexities of payment and reimbursements, ensuring that medical care service providers obtain compensation for their solutions efficiently and precisely
A thorough understanding of RCM includes recognizing the several parts that make it effective. Key facets consist of person scheduling, insurance policy verification, charge capture, claim entry, and settlement publishing. Each of these aspects requires thorough attention to information and robust systems to minimize mistakes that can bring about income loss. In addition, RCM is not only concerning monetary collections; it also aims to enhance individual fulfillment by lowering billing errors and boosting transparency.
The performance of RCM rests upon the smooth assimilation of technology and human resource proficiency. Using innovative software program options allows health care institutions to automate repeated tasks, consequently lowering administrative problems. Additionally, trained employees are essential in browsing regulative requirements and payer policies, ensuring compliance and maximizing profits recovery.
Enhancing Person Enrollment
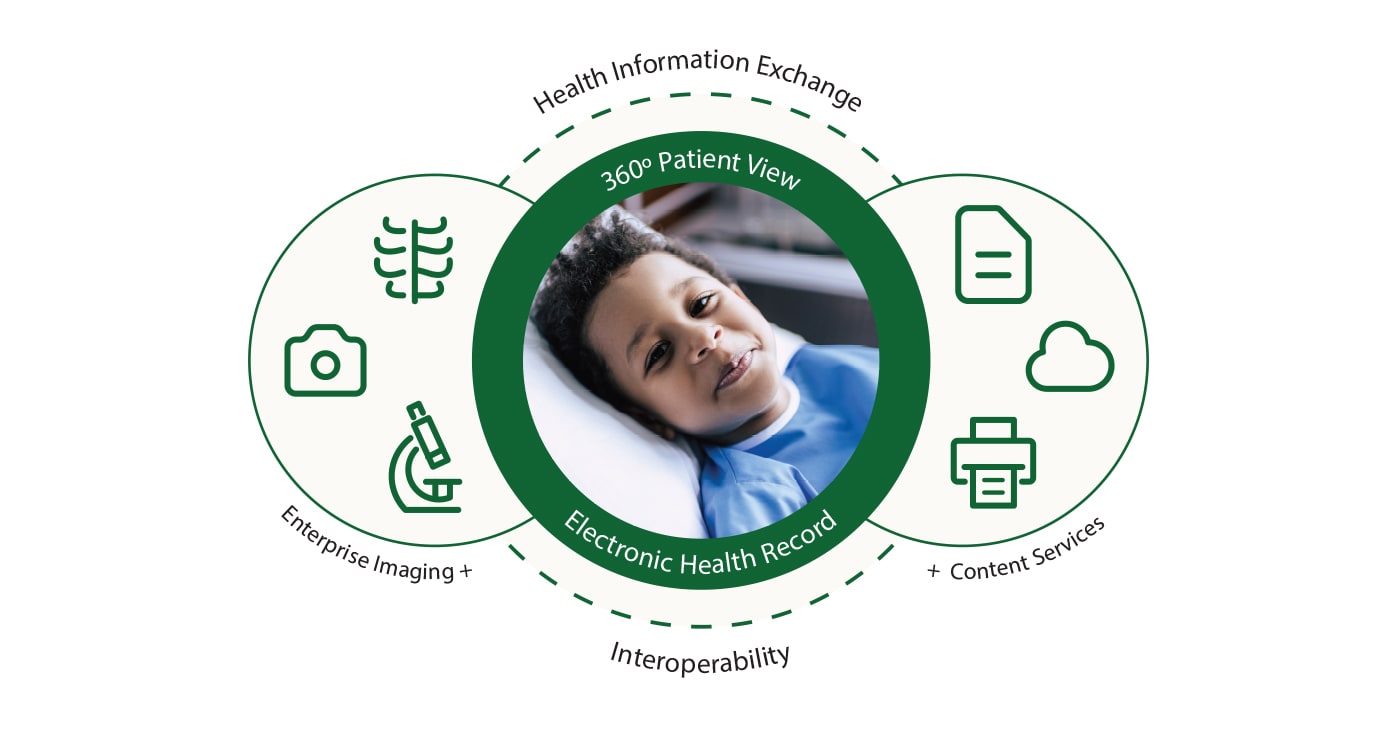
Streamlining patient enrollment is a fundamental action in improving the effectiveness of healthcare revenue cycle monitoring. It includes enhancing the preliminary interaction between individuals and doctor to ensure a smooth information collection process. Secret components consist of the accurate capture of person demographics, insurance verification, and authorization purchase. By digitizing these processes via integrated electronic health documents (EHR) systems, health care facilities can minimize errors, reduce documentation, and expedite individual throughput (Healthcare RCM).
Automated systems assist in verifying insurance eligibility in real-time, which not only reduces management problems however likewise boosts individual fulfillment by protecting against unforeseen billing concerns. Additionally, pre-registration processes allow people to full forms on-line before their browse through, lowering delay times and allowing staff to focus on more facility tasks. This aggressive strategy guarantees that all required information is collected and verified before treatment is given, consequently avoiding delays in succeeding billing and claims procedures.
Training team to use these systems successfully is important. It guarantees that data entrance is precise and constant, cultivating a seamless transition from client registration to other profits cycle procedures. Eventually, improving patient enrollment lays the foundation for a much more reliable, patient-centered health care shipment design.
Efficient Billing Solutions
Effective billing options are integral to enhancing medical care earnings cycle management. They work as the backbone for ensuring exact and timely financial purchases in between patients, medical care carriers, and insurance provider. By leveraging advanced innovation and structured processes, health care centers can considerably decrease invoicing errors, decrease delays, and enhance capital. Executing durable invoicing systems helps with exact charge capture, guaranteeing all services made are made up and billed appropriately. Automation devices can resolve invoicing information with scientific documents, avoiding and reducing inconsistencies case rejections.
Moreover, effective payment options encourage medical care companies to offer clear rates and invoicing details to individuals, promoting count on Visit This Link and improving client fulfillment. Real-time billing systems make it possible for medical care staff to give prompt comments on patient qualification and out-of-pocket costs, boosting the overall client experience. These remedies also permit smooth integration with electronic wellness records (EHR), making sure that invoicing and professional information are in sync, lowering management worries on medical care service providers.
Incorporating reliable billing services right into the earnings cycle management structure not only optimizes functional effectiveness yet additionally reinforces economic efficiency. By lessening mistakes, accelerating repayment cycles, and boosting patient interaction, healthcare companies can concentrate a lot more on supplying top quality treatment while preserving financial sustainability.
Optimizing Insurance Claims Processing
In the realm of medical care profits cycle administration, maximizing insurance claims handling is essential for keeping monetary health and operational effectiveness. A streamlined claims procedure minimizes the time in between service distribution and payment, therefore enhancing money flow and lowering the probability of mistakes. Effective claims refining begins with accurate documents and coding, which are necessary to make certain that cases are sent without inconsistencies that might lead to denials or hold-ups.
Leveraging sophisticated innovation, such as automated cases monitoring systems, can considerably improve the efficiency of this process. These systems are designed to automate repeated jobs, track claims through each phase, and flag potential issues early. This not just reduces the management worry on personnel yet also raises the accuracy of entries by minimizing human error.
Enhancing Income Collection

In addition, rejection monitoring plays a critical role in taking full advantage of revenue collection. Identifying patterns in insurance claim rejections, understanding root reasons, and implementing corrective actions can significantly decrease repeating problems, consequently boosting capital. Suppliers need to spend in durable analytics devices that facilitate thorough reporting and analysis, enabling them to fix and resolve rejection patterns immediately.
Timely follow-up on superior insurance claims is one more crucial element of profits collection. Establishing an organized method to keep an eye on and go after aged accounts makes certain that no profits is left unclaimed. Utilizing dedicated staff or automated systems to track these claims can enhance efficiency and ensure constant cash money inflows.
Verdict
Healthcare Earnings Cycle Monitoring (RCM) processes dramatically improve management performance by integrating advanced modern technology and human expertise (Healthcare RCM). The automation of patient registration, invoicing, and claims processing speeds up and minimizes mistakes money circulation, eventually boosting person fulfillment through real-time insurance coverage confirmation and clear payment. By guaranteeing smooth functional flow, RCM permits medical care carriers to focus on quality treatment while taking full advantage of revenue healing and keeping monetary security, thus transforming administrative jobs right into efficient, streamlined procedures
Revenue Cycle Management (RCM) in healthcare is a vital process that ensures the financial health of clinical organizations by looking after the my link whole lifecycle of individual service profits.Enhancing individual enrollment is a fundamental action in improving the performance of health care profits cycle management. It entails maximizing the first communication between clients and medical care service providers to make sure a smooth information collection process.Furthermore, reliable payment options equip medical care companies to offer transparent pricing and billing information to clients, fostering trust fund and enhancing person complete satisfaction. Real-time payment systems make it possible for medical care team to provide prompt comments on individual qualification and out-of-pocket expenses, boosting the overall patient experience.
Report this page